Effects of alcohol on migraine
The relationship between alcohol and headache is complex. As discussed above, alcohol can cause headaches as part of post intoxication syndrome of a hangover. Typically occurring within several hours of the cessation of drinking, hangovers generally consist of nausea, abdominal discomfort, headache and psychological symptoms. Frequent hangovers generally lead to worsening social, educational and employment functioning. The treatment of hangovers is fraught with mythology. It seems that everyone has a recommendation: from consumption of raw eggs, fat heavy foods, to coffee and more alcohol. There is little evidence supporting any of these interventions beyond the general recommendations of avoiding alcohol.
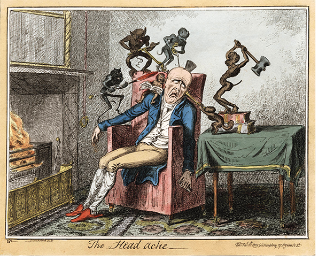
George Cruikshank, 1792-1878
Caricatures at the publication. Le Petit [circa 1835], Dublin.
Alcohol can also enact its effect on headache in other ways. Some migraine sufferers have found alcohol to be a direct trigger for their events, without waiting for the withdrawal period. Others have speculated that “darker alcohols” including red wine and certain distilled spirits may have a greater chance of inducing a migraine. But, the fact is that all alcohol has the risk of acting as a trigger. To date, no evidence has demonstrated that the tannins, sulfates or sulfites in commercial alcohol has any greater risk of being a migraine inducer.<br> <br>Several studies suggest that migraine sufferers are also at a greater risk of other headache subtypes. This may include tension type headache, hypnic headache, idiopathic headache, ice cream headache and hangover headaches. As yet, there has not been a blinded study to actually demonstrate that migraine sufferers are at greater risk of hangovers, but speculation runs rampant.<br> <br>It may be difficult to distinguish between migraine and hangover as several associated symptoms may also overlap - including worsening with movement and potentially disabling nausea. Following the International Classification of Headache Disorders criteria, migraine cannot be diagnosed when there are other possible causes for headache including substance induced toxicity, so these events could only be termed “migrainous” and not actually migraines. However, such hair splitting may be more significant to physicians and less important to individuals who simply want to feel better.
Joint studies with N1‑Headache™ conducted with The Migraine Trust and National Headache Foundation indicated the importance of environmental and social factors that are associated with the context of drinking alcohol. In fact, the context of drinking alcohol seems more important in determining an individual’s migraine risk than the alcohol itself and in these studies alcohol turned up as trigger only in a small minority of users. More surprisingly, alcohol was more often found as protectors.
For instance, in the Migraine Trust study, only 9 out of 154 users had one or the other type of alcohol as a trigger (less than 6%). But 33 users (21%) showed a protective association with alcohol. Interviews with users often underscored that drinking was in the context of relaxation: a glass of wine with their spouse, beer with friends. In one interesting example, a female N1‑Headache™ user who occasionally drank different types of alcohol showed no triggers associated with any type of alcohol, with the singular exception of sparkling wine. When asked what determined whether she drank sparkling wine versus other type of alcohols, she responded that she only drank sparkling wine at formal occasions - and quickly admitted that the formality and crowds caused her stress.

Alcohol as a Protective Factor?
Ms. M. is a 45 year old woman who had been tracking her headache triggers with N1‑Headache™ and was actually surprised to find that consumption of red wine was negatively
correlated with the risk of having a migraine that day. This led her to speculate whether a higher consumption
of alcohol may actually lead to fewer migraines. In tracking their headache triggers and protectors, other
individuals may actually be surprised to find alcohol consumption may actually be correlated with a lower risk
of a headache. However, this may actually represent an incompletely understood association. In further
analysis of Ms. M’s habits, it was noticed that she only consumed red wine when she was relaxed, in a positive
environment and felt she was able to safely consume alcohol. It was a situational use and that situation may
be what was associated with a lower risk of migraine. While she initially misattributed the protective effect
to alcohol, further assessment led to a more complete understanding of positive environmental and social
protectors.

Our conclusion? Obviously, it would be reasonable to expect individual variation of alcohol’s effects in migraine based on individual genetic variation of alcohol metabolism. Unfortunately, we have found no studies relating the genetic variation in alcohol metabolism and its possible effect in individuals with respect to alcohol as a migraine trigger. Recent studies that N1‑Headache™ conducted with The Migraine Trust and National Headache Foundation indicate alcohol is not by any means a common or even a consistent migraine trigger and therefore needs to be examined on an individual basis. In addition, the individual social context in which alcohol is consumed seems more important in determining an increased or decreased risk of a migraine attack. As a result, since most people seem to drink alcohol in relaxing situations – it is more commonly found associated as a protector. Nevertheless, other health effects of alcohol strongly suggest that if we drink, we should drink in moderation (and be relaxed and happy about it!).
Go back to articles





 Loading...
Loading...